Today is our topic of discussion Lymphatic filariasis
Lymphatic filariasis
Definition:
Filariasis is an infection with a parasitic worm that lives in the human lymph system.
Agent:
Wuchereria bancrofti.
Periodicity:
w bancrofti display a nocturnal periodicity; appear in large numbers at night and retreat from blood during day.
Life cycle:
Man is definitive host and mosquito is intermediate host. Life cycle is pictured below-
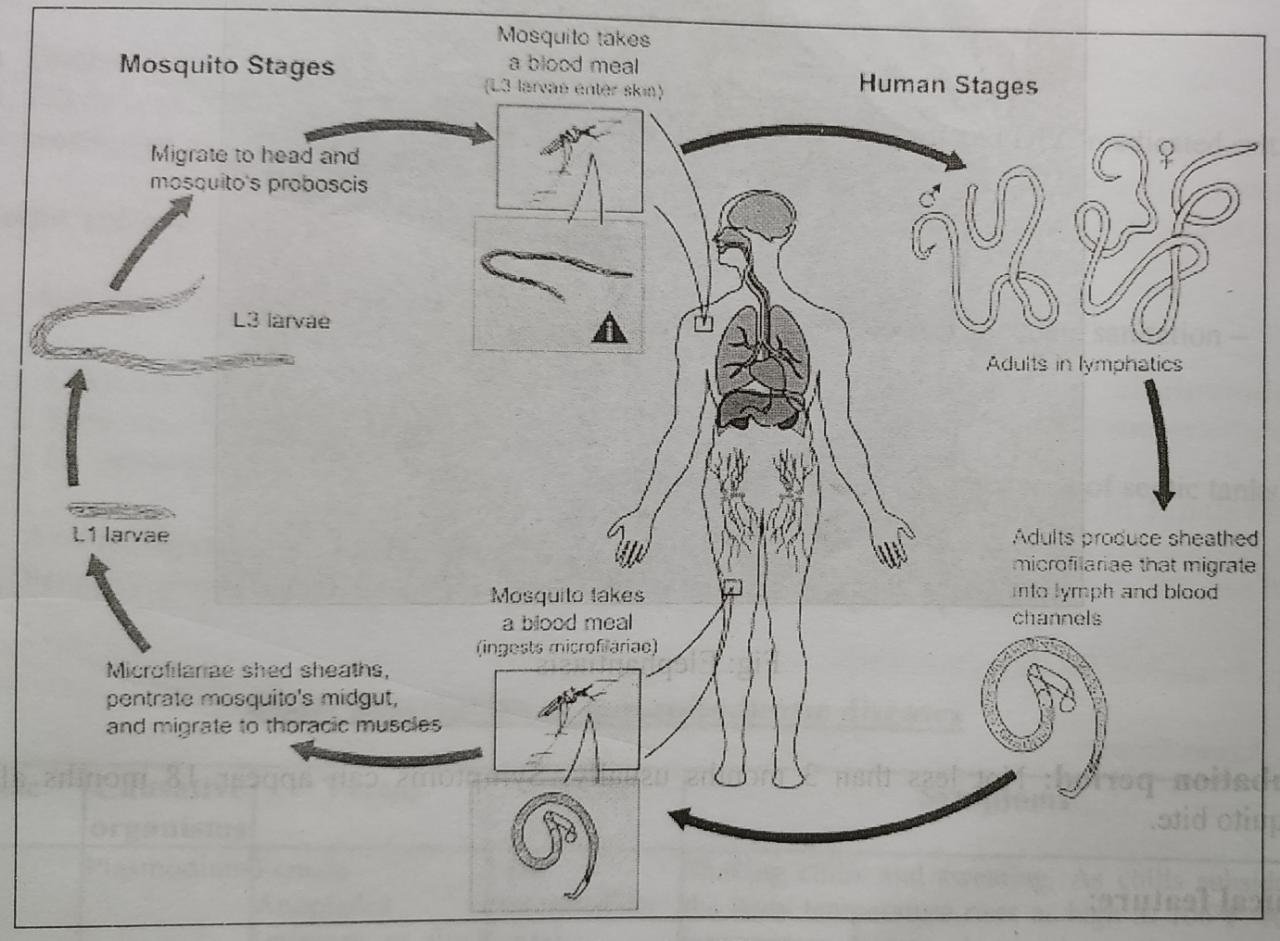
Fig: Life cycle of filaria
Reservoir of infection:
Person with circulating microfilaria in peripheral blood.
Host factors:
Age:
All ages are susceptible to infection.
Sex:
Higher in men.
Migration:
The movement of people from one place to another has led to the extension of filariasis into areas previously non-endemic.
Immunity:
Man may develop resistance to infection only after many years of exposure.
Social factors:
The disease often associated with urbanization, industrialization, migration of people, illeteracy, poverty and poor sanitation.
Vector:
Culex mosquito (Anopheles and Aedes mosquito can act as vector).
Environmental factors:
- Climate: Prevalence of Culex mosquito is seen in the temperature range of 22 to 38°C.
- Drainage: Lymphatic filariasis is associated with bad drainage system. Isolated
Mode of transmission:
Bite of infected vector mosquito
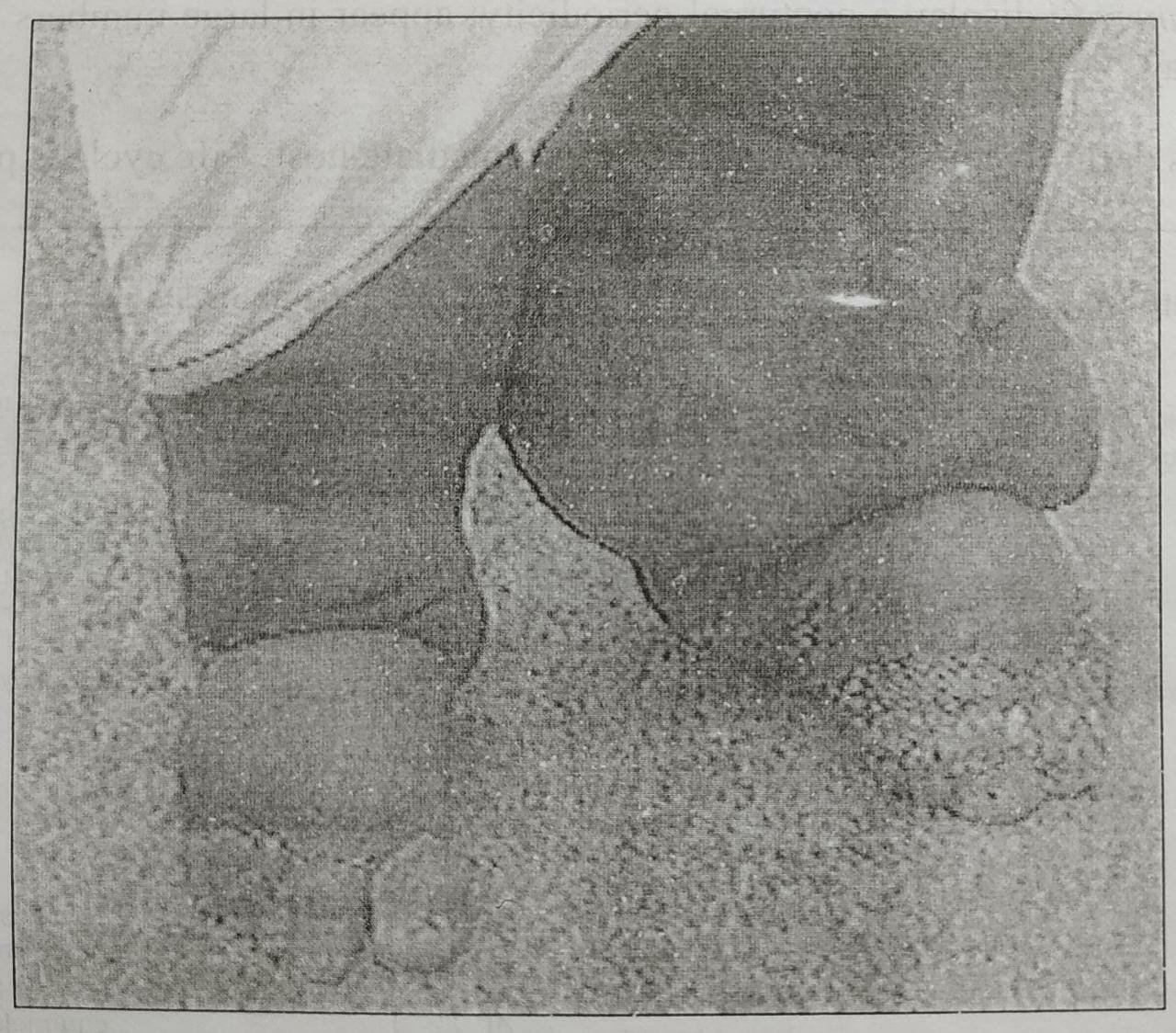
Fig: Elephantiasis
Incubation period:
Not less than 3 months usually. Symptoms can appear 18 months after a mosquito bite.
Clinical feature:
Lymphatic filariasis:
- Fever
- Erythema along the course of involved lymph vessels.
- Tissue damage: Restriction of flow of lymph → Swelling, scarring, and infections; legs and groin are most often affected →→→ Severe disfigurement, decreased mobility and long-term disability (elephantiasis).
- Hydrocele: Disfiguring enlargement of the scrotum.
Occult filariasis:
A lung condition called tropical pulmonary eosinophilia (TPE).
Treatment:
Anti-filarial drug:
Tab. Diethylcarbamazine (50 mg, 100 mg) 1 mg/Kg/day increasing to 6 mg/Kg/day over 3 days then continued for 3 weeks.
Prophylaxis:
Tab. Albendazole (400 mg)-yearly.
Skin care:
By soap and water to prevent secondary infection.
Elevation, exercises and pressure bandage:
To reduce swelling.

Control measure:
Chemotherapy:
a) Diethylcarbamazine (DEC) and albendazole.
b) Filaria control in the community: Mass therapy, selected treatment and DEC medicated salt.
c) Ivermectin
Vector control:
Anti-larval measures:
Elimination of breeding places by providing adequate sanitation –
- Chemical control.
- Removal of weeds.
- Environmental measure: Drainage of stagnant water and well maintenance of septic tanks.
Anti-adult measures:
Pyrethrum.
Personal prophylaxis:
Avoidance of mosquito bites by using mosquito nets.
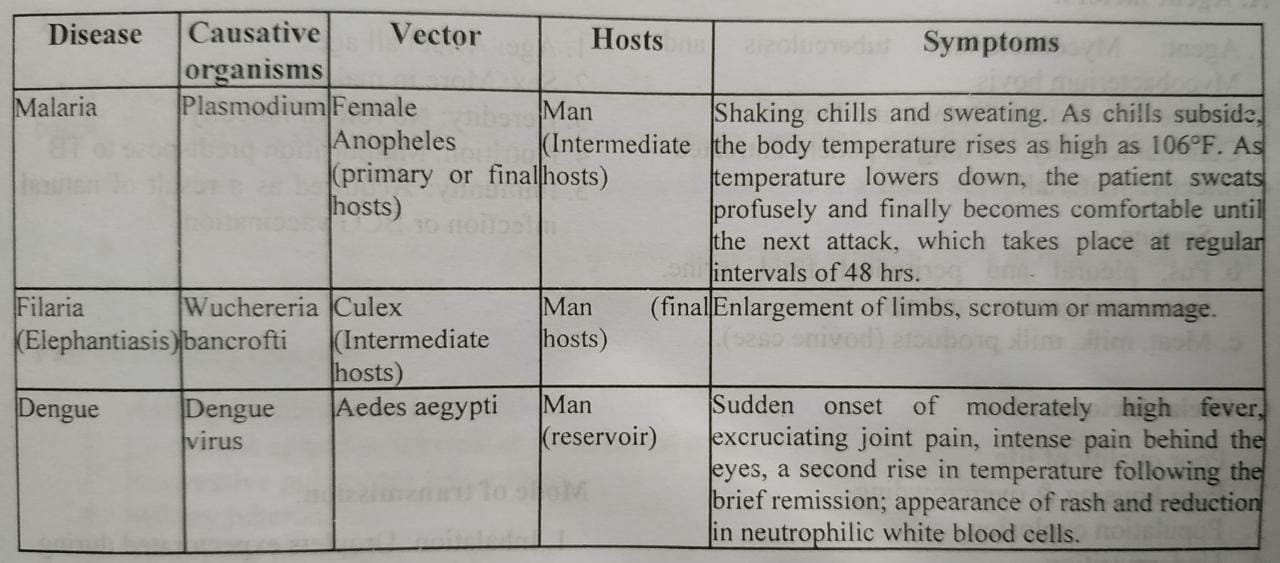
Short description of mosquito-borne diseases
See also :